Administering Intravenous Fluid Therapy
Select a Skill:
- » Preparing an Infusion Site
- » Performing Venipuncture
- » Dressing the Infusion Site
- » Troubleshooting Intravenous Infusions
- » Discontinuing Intravenous Therapy
Take the Review Test:

Safety
- Observe the Six Rights of Medication Administration.
- Know if the patient is right- or left-handed. For comfort and mobility, place an IV in the nondominant arm.
- Ensure that an IV system is intact, and there is no evidence of phlebitis or infiltration. An intact system ensures that you have maintained sterility and that no fluid or medication has been lost.
- Maintain sterility of a patent IV system using Infusion Nurses Society standards:
- Perform hand hygiene before and after palpating, inserting, replacing, or dressing any intravascular device.
- Use a catheter stabilization device that allows visual inspection of the access site.
- Replace short peripheral venous catheters, and rotate sites if clinical assessment indicates signs or symptoms of IV-related complications.
- Use each vascular access device only once for each insertion attempt.
- A single nurse should not make more than two attempts at initiating IV access. After two attempts, the nurse should have another nurse attempt the insertion.
Equipment
(Roll cursor over items to see labels)
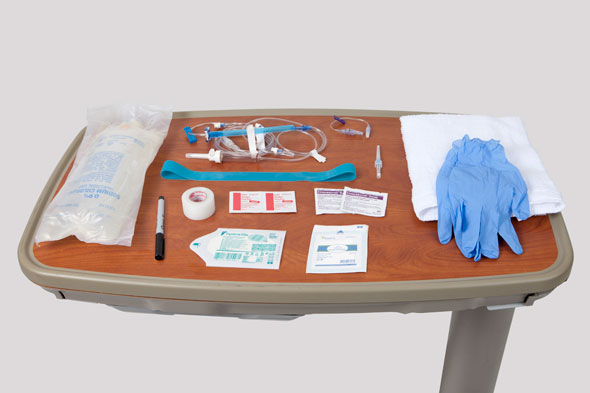
20- or 22-gauge catheter
IV Tubing
IV Extension set
IV Fluid
Waterproof pad or towel
2x2 gauze squares
Tourniquet
Tape
Clear, occlusive dressing
Clean gloves
Chlorhexideine swabs
Alcohol swabs
Delegation
The skill of initiating intravenous therapy may not be delegated to nursing assistive personnel (NAP). Delegation to licensed practical nurses (LPNs) varies by state Nurse Practice Act. Be sure to inform NAP of the following:
- Instruct NAP to notify you if the patient complains of any IV-related complications, such as pain, redness, swelling, or bleeding.
Preparation
- Review the accuracy and completeness of the health care provider’s orders for the type and amount of IV fluid, medication additives, infusion rate, and length of therapy.
- Follow the Six Rights of Medication Administration.
- Assess the patient’s knowledge of the procedure, reason for prescribed therapy, and arm placement preference.
- Assess for clinical factors/conditions that will respond to or be affected by administration of IV solutions:
- Body weight
- Clinical markers of vascular volume
- Clinical markers of interstitial volume
- Thirst
- Behavior and level of consciousness
- Determine if the patient is to undergo any planned surgeries or procedures.
- Assess laboratory data.
- Assess the patient’s history of allergies, especially to iodine, adhesive, and latex.
Follow-up
- Secure the IV device, and apply a sterile dressing over the site. (For details, see the Video Skill “Dressing the Infusion Site.”)
- Observe the patient every 1 to 2 hours or at established intervals per your agency’s policies and procedures for the following:
- Verify the type/amount of IV solution that has infused by observing the fluid level in the IV container.
- Check the infusion rate on the EID, or count the drip rate (if the solution is infusing by gravity).
- Check the patency of the vascular access device.
- Observe the patient for signs of discomfort during palpation of the vessel (over the transparent semipermeable membrane [TSM] dressing).
- Inspect the insertion site, noting its color, such as redness or pallor.
- Inspect the site for the presence of swelling, which is a sign of infiltration, or pain and tenderness, which is a sign of phlebitis. Feel the temperature of the patient’s skin above the dressing.
- Observe the patient to determine his or her response to therapy, such as laboratory values, I&O, weights, vital signs, and postprocedure assessments.
Documentation
- Record the number of attempts and sites of insertion.
- Precisely describe the insertion site, such as “cephalic vein on dorsal surface of right lower arm, 2.5 cm [1 inch] above wrist.”
- Document the method of infusion (gravity or electronic infusion device); type and rate of infusion; device identification number (if you are using an electronic infusion device); size, length, and brand of catheter; when the infusion began; and the patient’s response to the insertion. Use an infusion therapy flowsheet when available.
- Follow your agency’s policy for recording the patient’s status, IV fluid used, amount infused, and integrity and patency of the system.
- Report to the oncoming nursing staff: the type of fluid, flow rate, status of the vascular access device, amount of solution remaining in the infusion bag, expected time for completion of infusion and need to hang subsequent IV containers, and the patient’s condition.
- Report to the health care provider any signs and symptoms of IV-related complications.
Review Questions
1. Which action would the nurse perform to best ensure effective insertion of a venous access device into a patient’s arm?
 Anchor the vein by placing a thumb 1 to 2 inches below the site.
Anchor the vein by placing a thumb 1 to 2 inches below the site. Insert the device tip at a 45-degree angle distal to the proposed site.
Insert the device tip at a 45-degree angle distal to the proposed site. Place the patient’s left arm in a dependent position for 5 minutes before assessment.
Place the patient’s left arm in a dependent position for 5 minutes before assessment. Apply a tourniquet to the left antecubital fossa 8 to 12 inches above the proposed site.
Apply a tourniquet to the left antecubital fossa 8 to 12 inches above the proposed site.
2. How might the nurse prepare a patient to anticipate some discomfort when inserting a venous access device?
 Instruct the patient to expect a sharp, quick stick.
Instruct the patient to expect a sharp, quick stick. Insert the access device as quickly as possible.
Insert the access device as quickly as possible. Apply a topical anesthetic to the area before inserting the device.
Apply a topical anesthetic to the area before inserting the device. Promise that the procedure will not hurt once the device has been inserted.
Promise that the procedure will not hurt once the device has been inserted.
3. Which of the following technique(s) is/are best for minimizing a patient’s risk for injury when inserting a venous access device?
 Inserting the needle with the bevel up
Inserting the needle with the bevel up Using a vein on the dorsal surface of the arm
Using a vein on the dorsal surface of the arm Holding the skin taut directly below the site
Holding the skin taut directly below the site All of the above
All of the above
4. The nurse is inserting an over-the-needle catheter into a newly admitted patient. What will the nurse do after confirming blood return?
 Loosen or remove the tourniquet.
Loosen or remove the tourniquet. Advance the catheter 1 inch into the vein.
Advance the catheter 1 inch into the vein. Lower the catheter until it is flush with the skin.
Lower the catheter until it is flush with the skin. Thread the catheter into the vein up to the hub.
Thread the catheter into the vein up to the hub.
5. Which instruction might the nurse give to nursing assistive personnel (NAP) regarding the care of a patient with an intravenous access device?
 “Assess the IV site frequently for signs of inflammation.”
“Assess the IV site frequently for signs of inflammation.” “Be sure not to obscure the insertion site with the dressing.”
“Be sure not to obscure the insertion site with the dressing.” “Let me know when you notice that the IV bag contains less than 100 milliliters.”
“Let me know when you notice that the IV bag contains less than 100 milliliters.” “Explain the symptoms of infection to the patient.”
“Explain the symptoms of infection to the patient.”
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

