Managing Intravenous Fluid Therapy
Select a Skill:
- » Regulating an Intravenous Infusion
- » Using an Infusion Pump
- » Changing Intravenous Tubing and Fluids
- » Changing Intravenous Dressings
Take the Review Test:

Safety
- Be aware that changes in patient position, flexion of the intravenous (IV) site extremity, and occlusion of the IV device will influence infusion rates.
- Be aware that vasospasm, venous trauma, or manipulation of the device will also affect infusion rates.
- To achieve the best therapeutic outcome with the fewest complications, assess the IV system, infusion pump, and flow rate regularly, according to agency policy.
- A significant infiltration may occur before the infusion pump’s positive pressure alarm sounds. It remains necessary to do frequent IV site assessments.
- Although the use of electronic infusion devices (EIDs) has improved patient safety outcomes, the EID is not without the risk of malfunction, placing a patient at risk for harm or injury. Always check the manufacturer’s recommendations for specific device instructions.
- An anti‒free-flow valve safeguard will prevent a bolus infusion in the event of pump malfunction or removal of tubing from the pump flow channel.
Equipment
(Roll cursor over items to see labels)
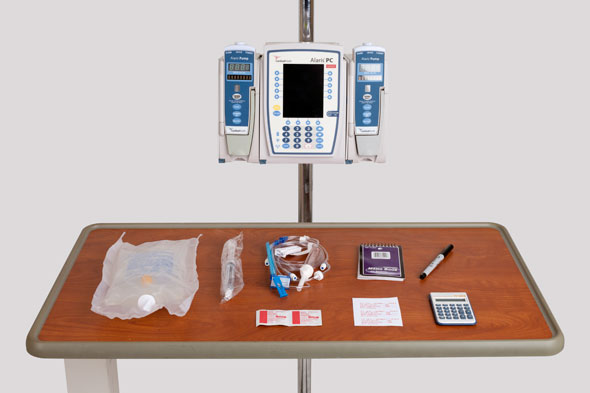
Calculator
Paper and pen
Label for IV solution
SMART Pump
Electroic infusion device (EID)
Extension tubing
IV fluid to be administered
Prefilled NS flush in syringe with 10 mL size barrel
Alcohol swabs
Delegation
The skills of regulating the intravenous (IV) flow rate and manipulating the settings on an electronic infusion device (EID) may not be delegated to nursing assistive personnel (NAP). Delegation to licensed practical nurses (LPNs) varies according each state’s nurse practice act. Before delegating related skills, be sure to inform NAP of the following:
- Instruct NAP to inform you when the EID alarm sounds.
- Instruct NAP to inform you when less than 100 mL remain in the the fluid container.
- Instruct NAP to report any patient complaints of discomfort related to the infusion, such as pain, burning, bleeding, or swelling at the insertion site.
Preparation
- Review the health care provider’s orders for accuracy and completeness; check the patient’s name; the solution type, volume, additives, and rate of infusion; and the duration of IV therapy. Follow the Six Rights of Medication Administration.
- Be aware that it is common for health care providers to write abbreviated IV orders, such as: “D5W with 20 mEq KCl/L 125 mL/hr continuous.” This order implies that the IV should be maintained at this rate indefinitely, until a subsequent order changes or discontinues the IV prescription.
- Assess the patient’s knowledge of the effect of IV site position on flow rate.
- Perform hand hygiene. Inspect the IV site for signs of IV-related complications, such as pain, swelling, and redness.
- Check the patency of the IV tubing and venous access device (VAD).
- Identify the patient’s risk for fluid and electrolyte imbalance, considering the type and amount of IV fluid being infused. Be aware that neonates and patients with a history of cardiac or renal disease are at increased risk.
Follow-up
- Monitor the IV infusion at least every hour, noting the volume of IV fluids infused and the current rate of infusion.
- Observe the patient for signs of fluid volume excess or deficit, as well as for signs of fluid and electrolyte imbalance.
- Evaluate the patient for signs of IV-related complications, such as infiltration, phlebitis, venous access device (VAD) occlusion, and obstruction in the infusion tubing.
- At the change of shift or when leaving on break, report the flow rate and the fluid volume remaining in the infusion to the nurse in charge or to the next nurse assigned to care for the patient.
Documentation
- Record the hourly rate of infusion and use of the electronic infusion device (EID), according to your agency’s policy.
- Record intravenous (IV) insertion site appearance according to the frequency specified by agency policy.
Review Questions
1. Which response might the nurse give to nursing assistive personnel (NAP) who reports that the alarm is sounding on a patient’s electronic infusion device?
 “Assess the IV site for signs of inflammation.”
“Assess the IV site for signs of inflammation.” “Be sure to change the dressing on the IV site.”
“Be sure to change the dressing on the IV site.” “I’ll check the IV site and pump.”
“I’ll check the IV site and pump.” “Turn off the alarm.”
“Turn off the alarm.”
2. How would the infusion of intravenous (IV) fluids be affected if the tubing were unintentionally dislodged from the chamber of the control mechanism of the electronic infusion device (EID)?
 The infusion would slow to a “keep vein open” rate.
The infusion would slow to a “keep vein open” rate.  The patient would receive a bolus of fluid.
The patient would receive a bolus of fluid.  The infusion would continue at the prescribed rate.
The infusion would continue at the prescribed rate.  The flow of fluid would stop.
The flow of fluid would stop.
3. A patient is prescribed 1000 mL of intravenous (IV) normal saline to run over 8 hours. The initial fluid is hung at 0800. How many milliliters of fluid will have infused by 1200?
4. The nurse calculates that the patient is to receive 125 mL of intravenous (IV) normal saline per hour. After programming the infusion pump to deliver at that rate, how would the nurse ensure accurate fluid administration?
 First verify that the fluid is dripping, and then check the level of fluid remaining in the container every hour.
First verify that the fluid is dripping, and then check the level of fluid remaining in the container every hour. Ask another nurse to assess the programming of the pump.
Ask another nurse to assess the programming of the pump. Set the pump alarm to sound when half of the fluid has infused.
Set the pump alarm to sound when half of the fluid has infused. Check the IV site for complications.
Check the IV site for complications.
5. Which information is not necessary for the nurse to include when documenting the use of an electronic infusion device (EID) for an intravenous infusion?
 Location of the insertion site
Location of the insertion site  Time at which the infusion began
Time at which the infusion began  Patient’s pulse and heart rate
Patient’s pulse and heart rate  Hourly volume flow rate of the infusion
Hourly volume flow rate of the infusion
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

