Infection Control
Select a Skill:
- » Establishing and Maintaining a Sterile Field
- » Adding Items to a Sterile Field
- » Pouring A Sterile Solution
- » Using a Prepackaged Sterile Kit
- » Performing Sterile Gloving
Take the Review Test:
Safety
- Gain the patient’s full cooperation, in order to minimize contamination of your work area.
-
Explain to the patient how you will perform the procedure and what he or she can do to avoid contaminating sterile items, such as avoiding sudden body movement, refraining from touching sterile supplies, and avoiding coughing or talking over a sterile area.
-
Teaching the patient before you perform a sterile procedure eliminates the need to talk during the procedure, which can cause air droplet contamination of a sterile area.
- Remain organized while performing any sterile procedure, and keep bedside surfaces clutter free.
-
If a sterile field comes into contact with a contaminated object, or liquid splatters onto the drape, causing a strike through, the field has been contaminated. Discontinue preparing the sterile field, and start over with new equipment.
-
If a sterile item falls off of the sterile field, open the package containing a new sterile item, and add this item to the field, unless the field has been contaminated.
- Remember that as the nurse, it is your responsibility to stop the procedure when a break in sterile technique occurs.
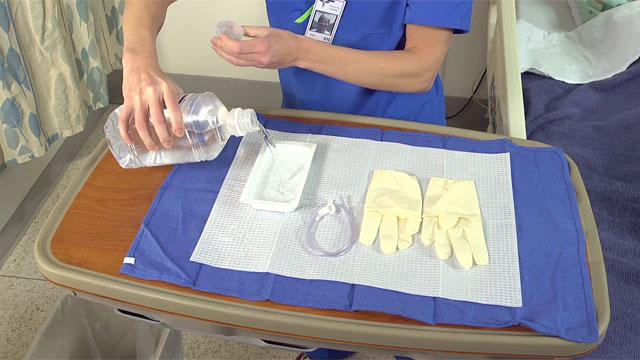
Equipment
(Roll cursor over items to see labels)
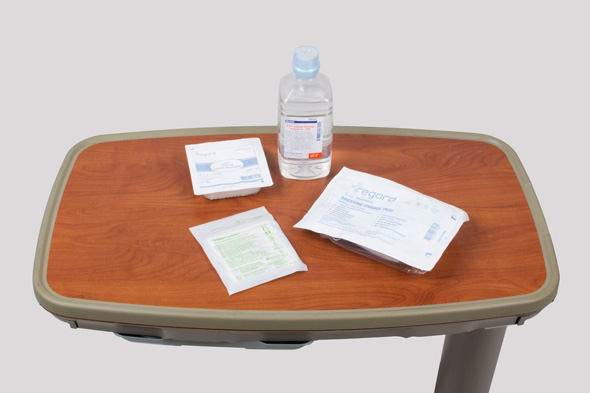
Sterile drape or kit that is to be used as a sterile field
Sterile drape or kit that is to be used as a sterile field
Sterile gloves
Sterile solution
Waist-high table/countertop surface
Delegation
The skill of pouring a sterile solution cannot be delegated to nursing assistive personnel (NAP). However, NAP may assist in positioning patients and obtaining extra supplies. Be sure to inform NAP of the following:
- Explain how to assist with patient positioning.
- Direct NAP to hand you any necessary supplies.
Preparation
- Verify that the procedure requires surgical aseptic technique.
- Check the integrity of the solution for discoloration, moisture, or any other signs of contamination.
- Verify the expiration date of the solution.
- Complete all other priority tasks, such as medication administration and suctioning the patient, before you begin the procedure.
- Prepare equipment to be used at the bedside.
Follow-up
- Watch for any breaks in sterile technique. Such a break requires that you set up a new sterile field.
Documentation
- No recording or reporting is required to establish a sterile field or to pour a sterile solution.
- Record the type of sterile procedure performed and the patient’s status.
Review Questions
1. When adding a sterile liquid to a sterile field, which action will contaminate the field?
 Extending your arm over the sterile field to pour the liquid into the receptacle
Extending your arm over the sterile field to pour the liquid into the receptacle Holding the bottle with the label facing the palm
Holding the bottle with the label facing the palm  Adding a liquid with a usable period that expires in 2 days
Adding a liquid with a usable period that expires in 2 days Placing the receptacle 1 inch (about 2.5 cm) from the edge of the sterile field
Placing the receptacle 1 inch (about 2.5 cm) from the edge of the sterile field
2. Which action is the most effective in minimizing the risk of contamination when using sterile liquids during a sterile procedure?
 Touch only the outer 1½ -inch margin of the sterile field unless you are wearing sterile gloves
Touch only the outer 1½ -inch margin of the sterile field unless you are wearing sterile gloves Avoid splashing when pouring sterile liquids onto the sterile field
Avoid splashing when pouring sterile liquids onto the sterile field Compare the label of the solution with the specific solution necessary for the procedure
Compare the label of the solution with the specific solution necessary for the procedure Assess the patient for any known allergies to the sterile solution
Assess the patient for any known allergies to the sterile solution
3. What direction would the nurse provide to nursing assistive personnel (NAP) assisting with a sterile procedure in which sterile solutions are being used?
 "Hand me that cup of water so I can pour it over my sterile field."
"Hand me that cup of water so I can pour it over my sterile field." "Would you please get me another bottle of sterile water?"
"Would you please get me another bottle of sterile water?" "Pour the sterile water into the container at the edge of the field.”
"Pour the sterile water into the container at the edge of the field.”  "Open the sterile water bottle and hold the label so that I can see it.”
"Open the sterile water bottle and hold the label so that I can see it.”
4. What would the nurse do if a sterile solution splashed onto a sterile field and contaminated the field during a dressing change?
 Complete the dressing change in a timely manner
Complete the dressing change in a timely manner Collect new supplies and prepare another sterile field
Collect new supplies and prepare another sterile field Move the lip of the bottle closer to the receptacle when pouring the remaining liquid
Move the lip of the bottle closer to the receptacle when pouring the remaining liquid Reposition the receptacle closer to the edge of the sterile field
Reposition the receptacle closer to the edge of the sterile field
5. When pouring a sterile liquid into a container on a sterile field, why does the nurse hold the bottle with the label facing the palm of the hand?
 The label is not sterile and will contaminate the field if it is splashed.
The label is not sterile and will contaminate the field if it is splashed. The label may become illegible if it is splashed.
The label may become illegible if it is splashed. The pour spout faces down when the bottle is held with the label facing the palm.
The pour spout faces down when the bottle is held with the label facing the palm.  The hand grips on the bottle are molded to fit correctly when the label is facing the palm.
The hand grips on the bottle are molded to fit correctly when the label is facing the palm.
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

