Preoperative Nursing Care
Select a Skill:
- » Performing a Preoperative Assessment
- » Promoting Family Support and Participation
- » Teaching Postoperative Exercises
- » Preparing a Patient for Surgery
Take the Review Test:

Safety
- Be aware that coughing may increase intracranial pressure, so is contraindicated after surgery on the brain, spine, or eye.
- If the patient cannot perform postsurgical exercises, document that staff or the primary caregiver must perform passive range-of-motion exercises every 2 hours while the patient is awake, or notify the surgeon and request an order for pneumatic compression cuffs.
- If the patient is unwilling to perform deep breathing, coughing, or turning exercises due to incisional pain, offer the patient pain medication 30 minutes in advance, or have the patient use the patient-controlled analgesia (PCA) device immediately before exercising.
- Be alert for shallow breathing and ineffective cough postoperatively, which could be signs of atelectasis or other pulmonary complications. Assess breath sounds, notify the health care provider, start ordered oxygen, and increase coughing exercises.
- If the patient develops postoperative circulatory complications, such as venous stasis or thrombophlebitis, notify the health care provider, rest and elevate the affected leg, and continue to exercise the unaffected leg.
Equipment
(Roll cursor over items to see labels)
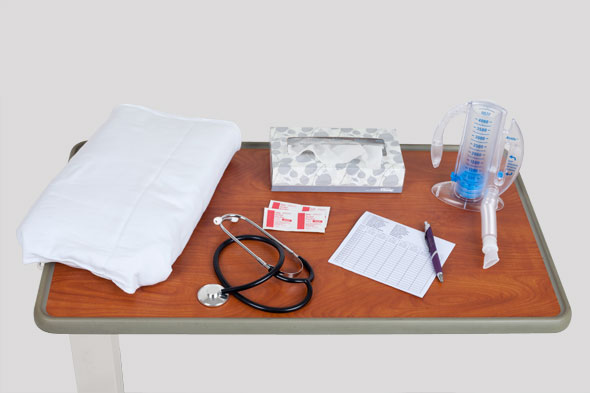
Pillow
Incentive spirometer
Alcohol pads
Stethoscope
Disposable tissues
Log for tracking breathing exercises
Delegation
The skill of teaching postoperative exercises may not be delegated to nursing assistive personnel (NAP). NAP may, however, reinforce your teaching and assist patients with postoperative exercises. Be sure to discuss the following with the NAP:
- Maintain precautions unique to the particular patient.
- Report if the patient is unable or unwilling to perform the exercises correctly.
Preparation
- Auscultate the patient’s lungs.
- Assess the patient’s ability to breathe deeply and cough. Place your hand on the patient’s abdomen, and have him or her take a deep breath. Note whether the patient moves the shoulders, chest wall, and abdomen. Measure the patient’s chest excursion during a deep breath. Ask the patient to cough into a tissue after taking a deep breath.
- Note the heightened risk for postoperative thrombus formation if the patient is elderly, immobilized, has a personal or family history of clot formation, or is a woman 35 years of age or older who smokes and takes birth control pills.
- To assess the risk of postoperative thrombus formation:
- Observe the patient’s calves for redness, swelling, warmth, and tenderness.
- Palpate the patient’s pedal pulses.
- Check for a Homans’ sign, that is, calf pain on foot dorsiflexion. Such pain is usually unilateral.
- Compare the legs for bilateral size equality.
- Assess the patient’s ability to move independently while in bed.
- Assess the patient’s willingness and ability to learn the exercises, noting factors such as attention span, anxiety level, level of consciousness, language skills, and pain.
- Assess the family caregiver’s willingness to learn and to support the patient postoperatively.
Follow-up
- Observe the patient performing all exercises independently.
- Observe the family caregiver’s ability to coach the patient.
- Evaluate the patient’s chest excursion.
- Auscultate the patient’s lungs.
- Gently palpate the patient’s calves for redness, warmth, swelling, and tenderness. Assess the patient’s pedal pulses.
- Monitor respiratory assessments for possible complications.
Documentation
- Record your physical assessment.
- Report and record any assessed patient complications and the action taken.
- Record which exercises you demonstrated to the patient and whether the patient can perform the exercises independently.
- Report to the nurse assigned to care for the patient during the next shift if the patient has any problem in practicing the exercises.
Review Questions
1. Why might a nurse teach a patient scheduled for surgery how to do postoperative exercises?
 To maximize a sense of well-being
To maximize a sense of well-being To minimize postoperative complications
To minimize postoperative complications To identify cultural factors that reflect the patient’s perception of pain
To identify cultural factors that reflect the patient’s perception of pain To evaluate the patient’s ability to participate in postoperative activities
To evaluate the patient’s ability to participate in postoperative activities
2. Before teaching a patient postsurgical exercises, the nurse premedicates the patient for pain. What benefit does this have specific to the patient’s learning?
3. What instruction might the nurse give to nursing assistive personnel (NAP) regarding postoperative exercises?
 “Find out if the patient has any language barriers.”
“Find out if the patient has any language barriers.” “Let me know when the patient actually begins exercising.”
“Let me know when the patient actually begins exercising.” “Please review a copy of the preoperative literature with the patient.”
“Please review a copy of the preoperative literature with the patient.” “Assess the method of learning the patient would prefer.”
“Assess the method of learning the patient would prefer.”
4. Which instruction might a nurse give a patient in order to protect a surgical incision when turning in bed?
 Hold your breath when turning.
Hold your breath when turning. Use a pillow to splint the incision.
Use a pillow to splint the incision. Take pain medication 30 minutes before turning.
Take pain medication 30 minutes before turning. Keep both legs straight when turning.
Keep both legs straight when turning.
5. The nurse is concerned that a patient will not be able to turn independently in bed after having surgery. What must the nurse do to help this patient?
 Reinstruct the patient in proper turning techniques.
Reinstruct the patient in proper turning techniques. Document that the patient refuses to turn independently.
Document that the patient refuses to turn independently. Communicate that the staff must turn the patient after surgery.
Communicate that the staff must turn the patient after surgery. Restrict turning unless absolutely necessary.
Restrict turning unless absolutely necessary.
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

