Vital Signs
Select a Skill:
- » Taking a Temperature
- » Assessing Radial Pulse
- » Assessing Apical Pulse
- » Assessing Apical-Radial Pulse
- » Assessing Respiration: Rate, Rhythm, and Effort
- » Obtaining Blood Pressure by the One-Step Method
- » Obtaining Blood Pressure by the Two-Step Method
- » Measuring Oxygen Saturation with Pulse Oximetry
- » Assessing Pain
- » Measuring Height and Weight
Take the Review Test:

Safety
- Know the patient’s medical history, types of therapies used, and medications, including over-the-counter (OTC) products. Many patients do not mention having used these because they fear being criticized or having the products taken away.
- Use nonopioids cautiously, since they may have more dangerous side effects than opioids, especially for older adults.
- Patients currently receiving opioids for chronic pain often require higher doses of analgesics to alleviate new or increased pain; this is tolerance, not an early sign of addiction. Be aware of individualized dosages, and ensure that all caregivers are aware of the dosages as well.
- Drug-drug interactions, including enhanced or reduced effects or side effects, often occur with the multiple drug use required by people with chronic pain. This practice is termed rational polypharmacy or multimodal analgesia.
- Communicate to the health care provider any significant changes in a patient’s comfort level and the need for changes in the patient’s pain management regimen.
- Know your agency’s policy for how often pain should be assessed and when follow-up assessments should be administered. During the first 24 hours on opioids, a patient requires frequent assessment, at least every 4 hours.
- Respiratory depression can be a side effect of any opioid, whether it is administered through the oral, IV, or epidural route, especially in an opioid-naïve patient. Using a standard sedation scale can prevent respiratory depression by allowing observation of and intervention for oversedation.
- While 0 is an ideal goal for a pain level, it is not a realistic goal in some patients with chronic/persistent pain. Many patients are able to do most of the things they wish to do at a pain intensity level of 1, 2, or even 3. If a patient’s goal is above 3, reassess his or her understanding of the pain scale.
Equipment
(Roll cursor over items to see labels)
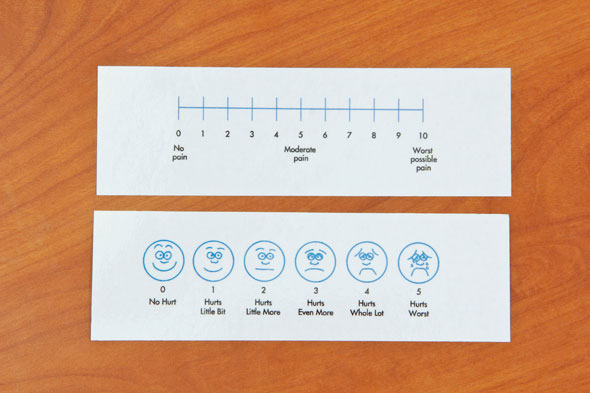
Pain Rating Scale (Numeric)
Pain Rating Scale (Faces)
Delegation
Pain assessment cannot be delegated to nursing assistive personnel (NAP). NAP may report patients’ comments or observations about their pain and provide selected nonpharmacological strategies, such as back massage, heat, cold, and elevation, per your instruction. Be sure to inform NAP of the following:
- How to eliminate environmental conditions that aggravate pain, such as excessive heat or noise in the room.
- How to provide maximum rest periods; a written schedule listing rest periods for all staff to follow is ideal.
- Turn and place the patient in a position of comfort at least every 2 hours, or remind the patient to turn himself or herself, using a pillow for splinting if needed.
- Observe for behavioral signs of pain in the patient who is unable to self-report. Such signs may include moaning, groaning, facial grimacing, or guarding.
- How to ask the patient to report the level of pain using the same pain-intensity scale chosen by the patient with you.
- Report to you immediately any patient’s report of pain intensity above the predetermined goal and any nonverbal behaviors suggestive of pain.
- Report to you immediately if they observe any signs of pain during patient transfer or other activities that may provoke pain.
Preparation
- Determine the patient’s risk for pain. Risk factors include having had an invasive procedure, having feelings of anxiety, and being unable to communicate their pain.
- Ask if the patient is in pain. Older adults and patients from certain cultural backgrounds may be reluctant to admit to having pain, and additional pain assessment techniques might need to be applied.
- Assess the patient’s previous responses to pharmacologic interventions.
- Assess the patient’s site of pain or discomfort.
- Assess verbal and nonverbal physical, behavioral, and emotional signs and symptoms of pain.
Follow-up
- Within 1 hour of an intervention (that is, when medication reaches its peak effect), ask the patient to describe his or her current level of relief, using a 0 to 10 scale.
- Compare the patient’s current pain level with the pain intensity goal he or she set.
- Compare the patient’s ability to function and perform the ADLs before and after any pain interventions.
- Observe the patient’s nonverbal behavior.
- Evaluate the patient for side effects of any analgesic administered.
Documentation
Record and report the following:
- Character of the patient’s pain before providing an intervention
- Therapies used
- Patient’s response to the interventions
- Inadequate pain relief:
- Reduction in the patient’s ability to function
- Adverse effects from pain interventions, both pharmacological and nonpharmacological
- Any patient or family education provided
- Report continued inadequate pain relief to health care provider.
Review Questions
1. A nurse is caring for a patient who has just had major abdominal surgery to resect a portion of his colon. What is the most reliable sign that the patient has significant postoperative pain?
 The patient rates his pain a 7 on a scale of 0 to 10.
The patient rates his pain a 7 on a scale of 0 to 10.  The patient winces and guards the area as the nurse gently palpates the abdomen.
The patient winces and guards the area as the nurse gently palpates the abdomen. The patient is having trouble sleeping and has become irritable.
The patient is having trouble sleeping and has become irritable.  The patient is moaning softly and frowning, with a pinched expression on his face.
The patient is moaning softly and frowning, with a pinched expression on his face.
2. What will the nurse instruct nursing assistive personnel (NAP) to do regarding the management of a patient’s pain?
 “Let me know at least 30 minutes before you transport her so I can administer her pain medication.”
“Let me know at least 30 minutes before you transport her so I can administer her pain medication.” “Be sure to keep the room temperature high and the TV on at all times.”
“Be sure to keep the room temperature high and the TV on at all times.” “Be sure to tell me if you notice grimacing, guarding, or any unusual behavior.”
“Be sure to tell me if you notice grimacing, guarding, or any unusual behavior.” “I’ve given her some medication; please report to me whether it seems to have relieved her pain within an hour or so.”
“I’ve given her some medication; please report to me whether it seems to have relieved her pain within an hour or so.”
3. Which observation indicates that a patient’s pain medication has been effective in managing pain that she rated a 6 out of 10 on a pain rating scale before the intervention?
 The patient is seen quietly reading a magazine.
The patient is seen quietly reading a magazine. The patient rates her current pain as 3 out of 10 on the pain rating scale.
The patient rates her current pain as 3 out of 10 on the pain rating scale. The patient is overheard telling her family that she is “feeling better today.”
The patient is overheard telling her family that she is “feeling better today.” The patient is observed sleeping, with a respiratory rate assessed at 18/minute, compared with 22/minute before the intervention.
The patient is observed sleeping, with a respiratory rate assessed at 18/minute, compared with 22/minute before the intervention.
4. A patient with a herniated disk is scheduled for surgery to fuse two vertebrae in her cervical spine. Which activity is most likely to be a palliative factor for this patient?
 Repainting her new apartment
Repainting her new apartment Lifting moving boxes on and off of a truck
Lifting moving boxes on and off of a truck Performing neck, back, and shoulder exercises prescribed by a physical therapist
Performing neck, back, and shoulder exercises prescribed by a physical therapist Performing yoga exercises from the patient’s favorite set of videotapes
Performing yoga exercises from the patient’s favorite set of videotapes
5. The nurse notices that his patient has none of the signs and symptoms normally associated with pain, such as diaphoresis, tachycardia, and hypertension. The patient does, however, seem moody and a bit uncooperative. What conclusion does the nurse draw?
 It is likely the patient is a drug seeker and has little or no pain.
It is likely the patient is a drug seeker and has little or no pain.  The patient’s problem is more mental than physical.
The patient’s problem is more mental than physical.  The absence of physiological signs and symptoms is associated with chronic pain.
The absence of physiological signs and symptoms is associated with chronic pain. The patient’s pain cannot be accurately assessed until the patient has been treated for anxiety.
The patient’s pain cannot be accurately assessed until the patient has been treated for anxiety.
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.


