Safe Medication Administration
Select a Skill:
- » Ensuring The Six Rights of Medication Administration
- » Administering Oral Medications
- » Documenting Medication Administration
- » Handling Medication Variations
- » Preventing Medication Errors
- » Using Automated Medication Dispensing Systems
Take the Review Test:

Safety
- Be aware that a medication error is more likely to occur at patient care transition points, such as during hospital admission, transfer from one unit to another, and discharge to home or another facility.
- If a patient questions the medication, stop and reevaluate the six rights of medication administration. An alert patient or family caregiver will know whether a medication is different from those received before.
- Minimize distractions and interruptions while preparing medication, including questions from staff and family, equipment alarms, and personal conversations.
- Read back all telephone orders and verbal orders for verification.
- Stay with the patient, and watch him or her take the medication.
- Prepare medications for one patient at a time.
- Administer only medications that you yourself have prepared. Do not ask another person to administer medications that you have prepared.
- Double-check all medication calculations and verify them with another nurse if unsure or if indicated according to agency policy.
- Question unusually large or small doses.
- Record allergy information for hospitalized patients on the front of the patient’s medical record and in the medication administration record (MAR). In addition, the patient should wear a band with all allergies listed.
- Encourage the health care provider to order medications that do not require splitting.
- Do not crush enteric-coated, long-acting, sustained-release, or sublingual medications. Refer to the “Do Not Crush List” issued by the Institute for Safe Medication Practices (ISMP) to ensure that a medication is safe to crush.
- Label all medications that require preparation and are not in their original containers. The label should include the drug’s name, strength, amount, and expiration date.
- Use different syringes for enteral and parenteral medication administration.
- When you administer insulin, a narcotic, a sedative, or an anticoagulant, follow current ISMP guidelines for administering high-alert medications. Be alert to look-alike/sound-alike medications.
- Consult the prescriber if you have any doubts about a medication order. Clarify illegible handwriting with the prescriber.
Equipment
(Roll cursor over items to see labels)
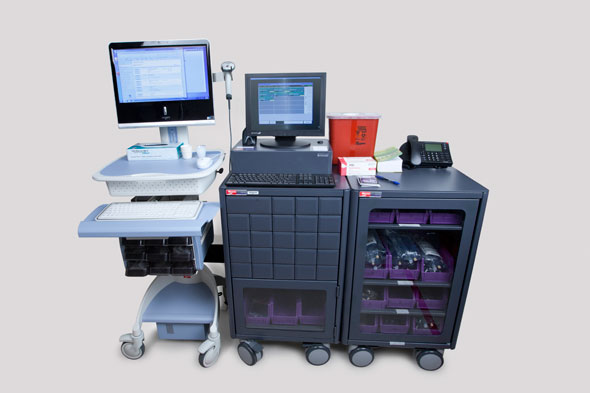
Medication cart or tray containing prescribed medication
Medication administration supplies: liquid dropper, syringe, soufflé cup
Medication administration record (MAR)
Clean gloves (if needed)
Delegation
The skill of ensuring the six rights of medication administration may not be delegated to nursing assistive personnel (NAP). Before delegating related skills, be sure to inform NAP of the following:
- Instruct assistive personnel to observe for potential side effects and to report their occurrence.
- Instruct assistive personnel to inform you if the patient’s symptoms (such as pain) are not relieved or continue to worsen after the medication is administered.
Preparation
- Perform hand hygiene before medication preparation.
- Minimize distractions while preparing medications.
- Make sure that the information on the medication administration record (MAR) corresponds exactly to the prescriber’s written order and with the label on the medication container.
- Identify the medication’s action, purpose, and side effects, and the nursing implications for administering the drug and monitoring the patient. Ensure that the medication order has not expired. Follow agency policy for renewing medication orders.
- Double-check all calculations and other high-risk medication administration processes (e.g., patient-controlled analgesia), and verify their accuracy with another nurse.
- When preparing medications, be sure that the label is clear and legible and that the drug has been properly mixed; has not changed in color, clarity, or consistency; and has not expired.
- Avoid touching tablets and capsules. Use sterile technique when preparing parenteral medications.
- Keep tablets and capsules in their wrappers, and open them at the patient’s bedside. Doing so allows you to review each medication with the patient. If a patient refuses a medication, there will be no question which one was withheld.
- Identify and obtain preadministration assessments (e.g., vital signs, review of laboratory results).
Follow-up
- Ensure that the patient understands the purpose of each medication. Teach the patient about the medication’s side effects, and describe the criteria for calling the nurse or physician.
- Evaluate the patient’s response after the administration of a PRN medication.
Documentation
- Record the medication’s name, actual time of administration, dose, route, and site location if appropriate on the MAR immediately after medication administration. For paper MARs, include your initials or signature as directed by agency policy.
- Do not chart medication administration until after the drug is taken by the patient. Note that some bar coding systems will document the time of administration at the point of delivery when scanned. (For details, see the Video Skill “Documenting Medication Administration.")
- Document the patient’s response to PRN medications.
- If a medication is refused, document that it was not given, the patient’s reason for refusal, and the time at which the health care provider was notified.
Review Questions
1. When preparing to administer a new medication, what would the nurse do first to ensure the patient’s safety?
 Perform hand hygiene.
Perform hand hygiene. Compare the written order with the medication administration record (MAR).
Compare the written order with the medication administration record (MAR). Inform the patient about the medication.
Inform the patient about the medication. Review appropriate nursing considerations.
Review appropriate nursing considerations.
2. What is the most important step the nurse can take to ensure that the patient is getting the correct medication?
 Assess the patient’s ability to swallow oral medications without difficulty.
Assess the patient’s ability to swallow oral medications without difficulty. Question the patient about his or her experience with this or similar medications.
Question the patient about his or her experience with this or similar medications. Compare the medication label with the MAR three times.
Compare the medication label with the MAR three times. Evaluate the patient’s understanding of the safety issues related to the specific drug.
Evaluate the patient’s understanding of the safety issues related to the specific drug.
3. Which statement or question best illustrates the nurse’s understanding of the role of nursing assistive personnel (NAP) in medication administration?
 “Does the patient need her pain medication?”
“Does the patient need her pain medication?” “Let me know if she complains of any nausea.”
“Let me know if she complains of any nausea.” “What is the quality of her pain now?”
“What is the quality of her pain now?” “Tell her she doesn’t have an order for the drug she’s asking for.”
“Tell her she doesn’t have an order for the drug she’s asking for.”
4. As the nurse is administering medication to a patient, the patient states, “I’ve never seen that pill before.” What is the nurse’s most appropriate response?
 Reassure the patient that the pharmacy sent the right medication.
Reassure the patient that the pharmacy sent the right medication. Tell the patient that it is probably a different brand than what he takes at home and not to worry.
Tell the patient that it is probably a different brand than what he takes at home and not to worry. Tell the patient that you will review the physician’s order to clarify any discrepancies.
Tell the patient that you will review the physician’s order to clarify any discrepancies. Tell the patient that the doctor probably ordered a new medication.
Tell the patient that the doctor probably ordered a new medication.
5. What is the nurse’s best response after noticing that the route of administration has been omitted from a medication order?
 Ask which route the patient prefers.
Ask which route the patient prefers. Immediately notify the prescriber to request that the order be completed.
Immediately notify the prescriber to request that the order be completed. Refer to a current drug book to determine the most commonly prescribed route.
Refer to a current drug book to determine the most commonly prescribed route. Contact the pharmacy to determine the most appropriate route for this patient.
Contact the pharmacy to determine the most appropriate route for this patient.
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

