Safe Medication Administration
Select a Skill:
- » Ensuring The Six Rights of Medication Administration
- » Administering Oral Medications
- » Documenting Medication Administration
- » Handling Medication Variations
- » Preventing Medication Errors
- » Using Automated Medication Dispensing Systems
Take the Review Test:

Safety
- Notify the health care provider if you suspect polypharmacy in the older adult.
- If administration of a medication is contraindicated based on patient assessment, hold the drug and notify the prescriber.
- If a patient questions a medication, stop and recheck the prescriber’s orders against the medication administration record (MAR) to be certain there is no mistake. An alert patient or family caregiver will know whether a medication is different from those he or she has received before.
- Keep tablets and capsules in their wrappers, and open them at the patient’s bedside. This allows you to review each medication with the patient. If a patient refuses a medication, there will be no question which one was withheld.
- If a patient refuses a medication, determine the reason and take appropriate action.
- If a medication error occurs, assess the patient’s condition and notify the health care provider immediately. Report all medication errors.
Equipment
(Roll cursor over items to see labels)
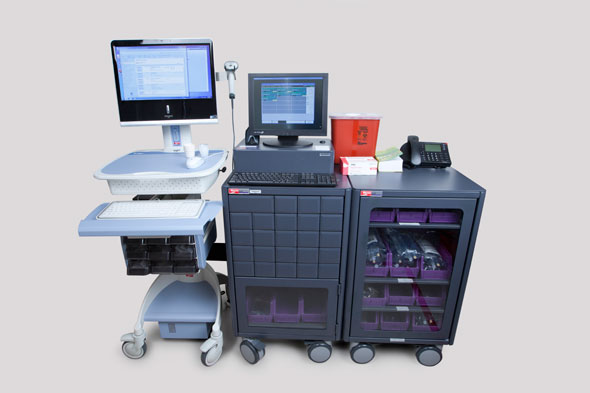
Medication cart or tray containing prescribed medication
Medication administration supplies
Medication administration supplies
Medication administration record (MAR)
Delegation
The skill of handling variations in medication administration may not be delegated to nursing assistive personnel (NAP). Before delegating related skills, be sure to inform NAP of the following:
- Instruct NAP to observe for side effects and to report their occurrence.
- Instruct NAP to inform you if the patient's symptoms (such as pain or itching) continue or worsen after the medication is administered.
Preparation
- Make sure that the information in the medication administration record (MAR) corresponds exactly with the prescriber’s written order and with the label on the medication container. Do not interpret illegible handwriting; clarify it with prescriber.
- Identify the medication’s action, purpose, side effects, and nursing implications for administering and monitoring. Ensure that the medication order has not expired.
- Review any preadministration assessments (e.g., vital signs, laboratory results).
- Assess for contraindications to or incompatibilities with the prescribed medication. Notify the prescriber if any exist.
- Read the label on the medication container and compare it with the MAR at least three times: before removing the container from the supply drawer, when placing the medication in an administration cup/syringe or taking it to the patient’s room, and just before administering the medication to the patient.
Double check all calculations and other high-risk medication administration processes (e.g., patient-controlled analgesia), and verify them with another nurse.
Follow-up
- Record medications immediately after administration (see agency policy). Include the drug name, dose, route, time, and your initials or signature.
- For medications that were held or refused, document the reason and notify the health care provider if appropriate.
- When a PRN medication is given for relief of symptoms, return to the bedside to assess the patient’s response to the PRN medication after an appropriate amount of time.
- Observe injection sites for bruising, bleeding, and inflammation, and respond to the patient’s complaints of localized pain or numbness.
Documentation
- Record the medication, dose, route, and time of administration on the MAR or computer printout immediately after administration. Include your initials or signature.
- If a narcotic is refused and discarded, document the narcotic waste according to facility policy, and include the signature of the nurse who witnessed the waste.
- If a medication is refused, document that it was not given, the patient’s reason for refusal, and the time at which the health care provider was notified.
- If a medication is held because of a contraindication, follow facility policy for documenting the withheld dose. Notify the health care provider if indicated, and record the time of notification and reason for withholding.
- For PRN medications, document the time, dose and route of administration in the MAR. Include the indication for giving the PRN medication. After waiting the appropriate amount of time, reassess the patient for response to the PRN medication and document the response.
Review Questions
1. As the nurse is at the bedside preparing to administer a new medication, the patient mentions that he is allergic to the drug. What will the nurse do first?
 Notify the physician
Notify the physician Withhold the medication
Withhold the medication Check to see if the patient is wearing a red allergy ID band
Check to see if the patient is wearing a red allergy ID band Review the medication administration record (MAR) for allergies
Review the medication administration record (MAR) for allergies
2. As the nurse prepares to administer oral acetaminophen, the patient refuses to accept the drug because it doesn’t look like the Tylenol she takes at home. After verifying that the medication and dosage are correct, what is the nurse’s best response?
 Informing the patient that the medication is a form of Tylenol
Informing the patient that the medication is a form of Tylenol Explaining that she will probably have increased pain if she refuses the medication
Explaining that she will probably have increased pain if she refuses the medication Showing the patient a picture of the medication
Showing the patient a picture of the medication  Explaining that drugs often come in different physical forms, depending on the manufacturer
Explaining that drugs often come in different physical forms, depending on the manufacturer
3. What is the nurse’s first response when a patient requests another dose of narcotic pain medication before it is time for the next dose?
 Consulting with the physical therapy department to arrange for a visit with the patient
Consulting with the physical therapy department to arrange for a visit with the patient Working with the patient to find alternative nonpharmacologic means of pain management
Working with the patient to find alternative nonpharmacologic means of pain management  Contacting the patient's provider to request an order for additional pain medication
Contacting the patient's provider to request an order for additional pain medication Giving the patient a detailed explanation of the need to limit the amount of narcotic medication she takes
Giving the patient a detailed explanation of the need to limit the amount of narcotic medication she takes
4. The patient has requested a PRN medication for nausea. Which of the following should the nurse do first?
 Offer dry crackers and ice chips if not contraindicated
Offer dry crackers and ice chips if not contraindicated Ask the patient about his allergies
Ask the patient about his allergies Explain the specific purpose of the medication
Explain the specific purpose of the medication Check to see when the medication was given last and make sure the time interval is up
Check to see when the medication was given last and make sure the time interval is up
5. After requesting a narcotic pain medication, the patient refuses it after the nurse prepares the injection. What is the nurse’s best initial response?
 Ask the patient the reason for his refusal
Ask the patient the reason for his refusal Notify the physician and asking for a different type of pain medication
Notify the physician and asking for a different type of pain medication Have another registered nurse witness the proper discarding of the drug
Have another registered nurse witness the proper discarding of the drug  Explain to the patient the need to manage pain effectively
Explain to the patient the need to manage pain effectively
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

