Safe Medication Administration
Select a Skill:
- » Ensuring The Six Rights of Medication Administration
- » Administering Oral Medications
- » Documenting Medication Administration
- » Handling Medication Variations
- » Preventing Medication Errors
- » Using Automated Medication Dispensing Systems
Take the Review Test:

Safety
- Be especially alert at patient care transition points, when medication errors are more likely to occur.
- Prepare medications using a “No Interruption Zone” to minimize distractions.
- Read back all telephone orders and other verbal orders for verification.
- If a patient questions the medication, stop and recheck it.
- Know the safe dosage range for each medication you administer.
- Record allergy information for hospitalized patients per agency policy. In addition, the patient should wear a color-coded allergy band. Never give a patient a medication when there is a known allergy.
- Do not crush an enteric-coated, long-acting, or sustained-release tablet or capsule. Refer to the “Do Not Crush List” issued by the Institute for Safe Medication Practices (ISMP). Place the medication between two medication cups or in a plastic sheath before using a pill crusher.
- Label any medication that requires preparation away from the patient’s bedside and is not in its original container.
- Do not use a parenteral syringe for oral or enteral liquid medications.
- Never assume that an ordered medication is the correct one or in the correct dose.
- Comply with the Joint Commission’s and ISMP’s “Do Not Use” and “Error Prone” list of abbreviations, acronyms, symbols, and dose designations. Be aware of “look-alike” and “sound-alike” drugs.
- Administer only medications that you have prepared. Do not ask another person to administer medications you prepare. Prepare medications for one patient at a time.
Equipment
(Roll cursor over items to see labels)
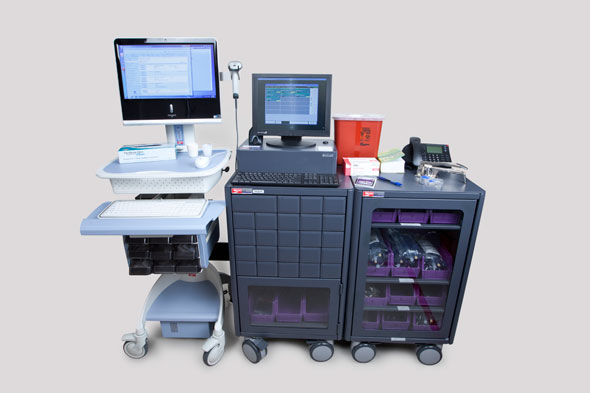
Medication cart or tray containing prescribed medication
Medication administration supplies
Medication administration supplies
Medication administration record (MAR)
Delegation
The skill of preventing medication errors may not be delegated to nursing assistive personnel (NAP). Nevertheless, it is the responsibility of the entire health care team to take steps to prevent medication errors, such as not talking while medications are being prepared. Before delegating related skills, be sure to inform NAP of the following:
- Instruct NAP to observe for potential side effects and to report their occurrence.
- Instruct NAP to inform you if the patient’s symptoms (such as pain or itching) continue or worsen after a PRN medication is administered.
Preparation
- Make sure that the information on the medication administration record or MAR corresponds exactly with the prescriber’s written order.
- Ensure that the medication order has not expired. Follow agency policy for medication order renewal.
- Minimize distractions during medication preparation. Close the door of the medication room, and do not perform other tasks while preparing a medication.
- Double-check all math calculations and other high-risk medication administration processes (e.g., patient-controlled analgesia), and verify them with another nurse.
- Assess the patient for contraindications to medications prior to administration.
- Review any preadministration assessments (e.g., vital signs, laboratory results).
- When preparing medications, be sure the label is clear and legible and that the drug has been properly mixed; has not changed in color, clarity, or consistency; and has not expired.
- Keep tablets and capsules in their wrappers, and open them at the patient’s bedside.
Follow-up
- Stay with the patient until all medications have been taken.
- Attend in-service programs on the medications you commonly administer.
- If an error occurs, report it to the nurse in charge, the health care provider, or other person as required by agency policy. Intervene as appropriate, such as administering an antidote, withholding the next dose, or monitoring the patient.
- Report all adverse reactions and side effects to the prescriber to ensure that such a sign is not incorrectly interpreted as a less serious adverse reaction.
Documentation
- Report all medication errors, including near misses and mistakes that do not cause obvious or immediate harm. Include the medication given, who was notified, the drug’s observed effects, and follow-up measures taken.
- Record the medication’s name, actual time of administration, and the dose and route on the MAR immediately after medication administration. Include your initials or signature. Do not chart medication administration until after the drug is given to the patient. (For details, see the Video Skill “Documenting Medication Administration.”)
- Follow agency policy for documenting medications that were held or refused. (For details, see “Handling Variations in Medication Administration.”)
- Complete an incident report within 24 hours. Document any call to the patient’s health care provider to clarify a medication order or request a change in a medication order.
Review Questions
1. When is a patient at a higher risk for a medication administration error?
 During a care transition point, such as transfer to another unit
During a care transition point, such as transfer to another unit While on a hospital unit for an extended length of time
While on a hospital unit for an extended length of time On the third postoperative day
On the third postoperative day When taking an active role in self-administration of insulin
When taking an active role in self-administration of insulin
2. As the nurse is giving a patient his medications, he remarks, “I’ve never seen this blue pill before.” What is the nurse’s correct response?
 “I’m sure the doctor knows what he’s doing. Don’t worry.”
“I’m sure the doctor knows what he’s doing. Don’t worry.” “Our pharmacy probably sent a generic form of what you’re used to taking.”
“Our pharmacy probably sent a generic form of what you’re used to taking.”  “What color pill are you used to seeing?”
“What color pill are you used to seeing?” “Don’t take it. Let me double-check the doctor’s order to make sure this is the correct medication for you.”
“Don’t take it. Let me double-check the doctor’s order to make sure this is the correct medication for you.”
3. What is the best way for the nurse to ensure that the patient does not receive the wrong dose because of a calculation error?
 Ask the pharmacy to calculate the correct dosage.
Ask the pharmacy to calculate the correct dosage. Consult a current drug book to determine the new dosage.
Consult a current drug book to determine the new dosage. Defer the calculation process to the provider.
Defer the calculation process to the provider. Ask another registered nurse to verify the calculation.
Ask another registered nurse to verify the calculation.
4. Which of the following nursing actions will reduce the risk of “wrong route” when administering a medication?
 Only splitting pills or tablets that have been prescored by the manufacturer
Only splitting pills or tablets that have been prescored by the manufacturer Using an oral dosing syringe when administering oral liquid medication
Using an oral dosing syringe when administering oral liquid medication Transcribing a fractional dose of less than one with a leading zero (e.g., 0.5 mg)
Transcribing a fractional dose of less than one with a leading zero (e.g., 0.5 mg) Crushing an oral medication that is difficult to swallow
Crushing an oral medication that is difficult to swallow
5. What is the most appropriate way for the nurse to split an unscored tablet?
 Use a pill-splitting device to split an unscored pill in half.
Use a pill-splitting device to split an unscored pill in half. Ask the pharmacy if it is appropriate to split the pill and if so, ask them to split and repackage it with the adjusted dose given on the label.
Ask the pharmacy if it is appropriate to split the pill and if so, ask them to split and repackage it with the adjusted dose given on the label. Use scissors to cut the pill in half.
Use scissors to cut the pill in half. Administer a whole pill every other day instead of every day.
Administer a whole pill every other day instead of every day.
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

