Injections
Select a Skill:
- » Preparing Injections from an Ampule
- » Preparing Injections from a Vial
- » Preparing and Administering Insulin
- » Drawing up More Than One Type of Insulin
- » Administering Intradermal Injections
- » Administering Subcutaneous Injections
- » Administering Intramuscular Injections
Take the Review Test:

Safety
- Ensure that the six rights of medication administration are followed: right medication, right dose, right patient, right route, right time, and right documentation.
- Be aware that the timing of insulin injection is critical to correct administration. Nurses need to know the onset, peak, and duration of all insulin given.
- If insulin has been stored in the refrigerator, bring it to room temperature before administering it.
- Visually inspect the vial of insulin before administration. Do not use the insulin if you note clumping, frosting, precipitation, altered clarity, or altered color.
- Do not interchange insulin types unless approved by the prescriber.
- Since insulin is considered a “high-alert” medication, have another registered nurse double-check the type and amount after it has been drawn up into the syringe and before administration.
- Do not mix insulin glargine (Lantus®) or insulin detemir (Levemir®) with any other types of insulin, and do not administer either intravenously.
Equipment
(Roll cursor over items to see labels)
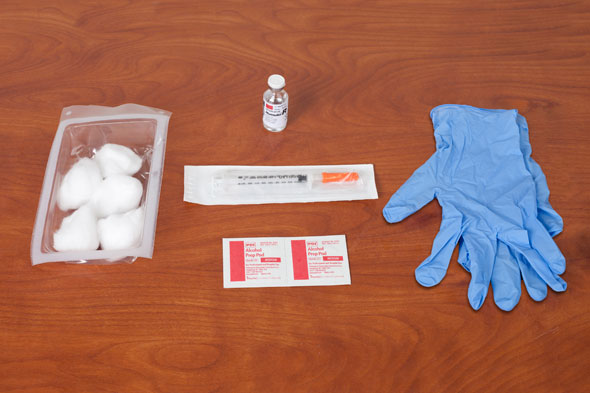
Vial of insulin
Subcutaneous U-100 insulin syringe (1 mL) with 29 gauge, 1/2 inch needles
Cotton balls
Alcohol swabs
Clean gloves
Delegation
No part of insulin preparation or administration may be delegated to nursing assistive personnel (NAP).
Preparation
- Check the accuracy and completeness of each medication administration record (MAR) against the health care provider’s orders. Confirm the patient’s name, the specific type of insulin, the dosage in units, and the time of administration. Clarify incomplete or unclear orders with the health care provider.
- Note if the patient has allergies.
- Determine the region in which previous insulin injections have been given, and plan to use a different site within the same region. Insulin is most quickly absorbed from the abdominal site and most slowly absorbed from the thighs.
- Obtain the patient’s current blood glucose level before preparing insulin.
- If insulin has been stored in the refrigerator, bring it to room temperature before administering it in order to prevent injection site irritation. Vials currently being used may be kept at room temperature.
- Draw up the appropriate dose of insulin into the insulin syringe. Check the label of the insulin and the amount drawn into the syringe against the MAR two times. Check the expiration date on the vial.
- Roll an insulin suspension preparation between your palms before drawing it up into the syringe.
- Coordinate the administration of rapid- and short-acting insulin with mealtime. Rapid-acting insulin is administered no more than 5 to 15 minutes before a meal. Short-acting insulin is administered no more than 20 to 30 minutes before a meal.
Follow-up
- Make sure that meal tray is delivered on time.
- Be alert for hypoglycemic reactions.
- Teach the patient about insulin storage, handling, and mixing (if appropriate), injection site rotation, self-injection, and blood glucose monitoring. Observe the patient’s demonstration of self-care techniques.
Documentation
- It is not necessary to document the preparation of insulin separately.
- For correction scale (sliding scale) insulin, record the blood glucose reading obtained before insulin administration.
- Record insulin administration in the MAR including site of injection.
- Document patient teaching regarding insulin preparation and administration and the patient’s response to teaching.
Review Questions
1. How can the nurse best ensure the patient’s safety when preparing insulin for administration?
 Obtain the patient’s current blood glucose level.
Obtain the patient’s current blood glucose level. Clean the injection site with an antibacterial swab.
Clean the injection site with an antibacterial swab. Apply clean gloves.
Apply clean gloves. Wipe the rubber seal of the vial with alcohol.
Wipe the rubber seal of the vial with alcohol.
2. How would the nurse prepare insulin to ensure its efficacy?
 Do not allow refrigerated insulin to warm up before administering it.
Do not allow refrigerated insulin to warm up before administering it. Follow aseptic technique during the entire process.
Follow aseptic technique during the entire process. Roll the vial of insulin suspension between the palms prior to drawing up the medication.
Roll the vial of insulin suspension between the palms prior to drawing up the medication. Monitor the patient’s blood glucose level before administering the injection.
Monitor the patient’s blood glucose level before administering the injection.
3. When will a patient’s blood glucose levels be most affected by a short-acting insulin injection, such as Humulin-R?
4. Which of the following statements is accurate regarding insulin administration?
 Vials of insulin may be stored in the freezer to extend their shelf life.
Vials of insulin may be stored in the freezer to extend their shelf life. If the rapid-acting insulin ordered is unavailable, it is safe to substitute an alternative rapid-acting insulin.
If the rapid-acting insulin ordered is unavailable, it is safe to substitute an alternative rapid-acting insulin. Vials of insulin must be inspected before each use for changes in appearance.
Vials of insulin must be inspected before each use for changes in appearance. All insulin must be shaken before use to redistribute particles within the suspension.
All insulin must be shaken before use to redistribute particles within the suspension.
5. To prevent hypoglycemia and enhance efficacy, it is appropriate to give rapid-acting insulin how many minutes before the next meal?
 5 to 15 minutes
5 to 15 minutes 30 to 40 minutes
30 to 40 minutes 60 to 90 minutes
60 to 90 minutes The timing of insulin around meals is not necessary.
The timing of insulin around meals is not necessary.
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.


