Respiratory Care and Suctioning
Select a Skill:
- » Ensuring Oxygen Safety
- » Setting Oxygen Flow Rates
- » Applying a Nasal Cannula or Face Mask
- » Maintaining an Airway
- » Providing Tracheostomy Care
- » Performing Oropharyngeal Suctioning
- » Performing Nasotracheal and Nasopharyngeal Suctioning
Take the Review Test:

Safety
- Be prepared to quickly reapply supplemental oxygen if the pulse oximetry (SpO2) level falls or if respiratory distress develops during suctioning.
- Keep the catheter in a nonairtight container, such as a brown paper bag or a plastic bag attached to a bed rail or in the suction canister area. Do not store the catheter where it will come into contact with secretions or excretions, which promote bacterial growth.
- Observe the principles of clean technique.
- Be careful using a Yankauer tip in older adults and in patients who have had recent oral or head/neck surgery.
Equipment
(Roll cursor over items to see labels)
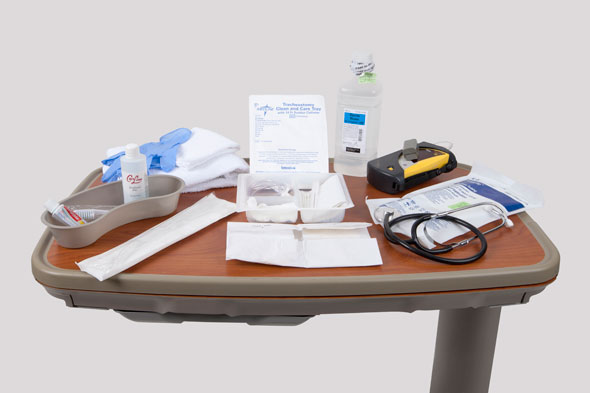
Stethoscope
Pulse oximeter
Clean gloves
Suctioning Kit
- Basin
- Sterile gloves
- Sterile drape
- Cotton balls
- Sterile swabs
1 L bottle sterile water
Suction tubing
Yankauer suction catheter
Washcloth and Towel
Oral hygiene supplies
Delegation
The skill of performing oropharyngeal (Yankauer) suctioning may be delegated to nursing assistive personnel (NAP). Do not routinely delegate this skill in the immediate postoperative period for a patient who has had oral or neck surgery. The nurse is responsible for assessing the patient’s respiratory status. Be sure to communicate the following with the NAP:
- Review appropriate suction limits for oropharyngeal suctioning, such as the appropriate suction pressure, expected frequency of suctioning, and the expected color and volume of secretions, for a particular patient.
- Discuss the risks of applying excessive or inadequate suction pressure.
- Caution NAP to avoid applying suction to mouth sutures or sensitive tissues, and to be careful not to dislodge tubes in the patient’s nose or mouth.
- Remind NAP to avoid stimulating the gag reflex.
- Advise NAP to report immediately any changes in the patient’s vital signs or pulse oximetry, or any sign of bloody sputum, difficulty breathing, or discomfort during or after the procedure.
Preparation
- Identify risk factors for airway obstruction, such as impaired cough or gag reflex, weakened respiratory muscles, impaired swallowing, and decreased level of consciousness.
- Assess for the following:
- Hypoxia (low oxygen utilization at the cellular or tissue level)
- Hypoxemia (low oxygen tension in the blood)
- Hypercapnia (elevated carbon dioxide tension in the blood)
- Apprehension, anxiety, decreased ability to concentrate, lethargy, decreased level of consciousness, increased fatigue and dizziness, irritability, tachycardia, tachypnea, decreased depth of breathing, elevated blood pressure, cardiac dysrhythmias, pallor, cyanosis, dyspnea, and use of accessory muscles for breathing.
- Use pulse oximetry to measure the patient’s oxygen saturation level (SpO2). Keep the oximeter in place.
- Determine the patient’s ability to hold or manipulate the catheter and his or her knowledge about the use of the suction catheter and the procedure.
- Assess for signs and symptoms of upper airway obstruction, such as gurgling on inspiration or expiration, restlessness, drooling, gastric secretions or vomitus in the mouth, or coughing without clearing secretions from the upper airway.
- Auscultate for adventitious sounds.
- Explain to the patient how the procedure helps clear airway secretions and relieves some breathing problems. Explain that coughing, gagging, or sneezing is normal and lasts only a few seconds. Encourage the patient to cough out secretions, and show him or her how to splint painful areas during the procedure. Practice coughing if the patient is able to do so.
- Position the patient in the semi-Fowler’s or sitting position. Place a towel, cloth, or drape across the patient’s neck and chest.
Follow-up
- Compare your assessment findings before and after the procedure.
- Auscultate the chest and airways for adventitious sounds.
- Inspect the mouth for any vomitus.
- Obtain the patient’s postsuction SpO2, and compare it with the presuction level.
- Watch the patient or a family member perform Yankauer suctioning, and suggest any necessary modifications in technique.
Documentation
- Record the amount, consistency, color, and odor of secretions; the number of times suctioned; the patient’s response to suctioning; and presuction and postsuction cardiopulmonary assessment findings.
- Record instructions given to any caregivers, and note their ability to perform the procedure correctly.
- Report any unresolved outcomes, such as worsening respiratory distress, to the health care provider.
Review Questions
1. Which action would the nurse perform when preparing to suction a patient’s oropharynx?
 Apply sterile gloves.
Apply sterile gloves. Place the patient in a semi-Fowler's or sitting position.
Place the patient in a semi-Fowler's or sitting position. Remove the nasal cannula.
Remove the nasal cannula. Flush the suction catheter with 200 mL of warm tap water.
Flush the suction catheter with 200 mL of warm tap water.
2. After oropharyngeal suctioning, what does the nurse do with the supplies?
 Place the Yankauer catheter in a clean, dry area.
Place the Yankauer catheter in a clean, dry area. Place all disposable equipment into the wrapper of the suction catheter before discarding it in a trash receptacle.
Place all disposable equipment into the wrapper of the suction catheter before discarding it in a trash receptacle. Fold the paper drape with the outer surface inward, and dispose of it in a biohazard receptacle.
Fold the paper drape with the outer surface inward, and dispose of it in a biohazard receptacle. Place dirty gloves in the biohazard receptacle in the patient’s room.
Place dirty gloves in the biohazard receptacle in the patient’s room.
3. When preparing to suction a patient’s oral cavity, why would the nurse first suction a small amount of water through the catheter?
 To moisten the exterior of the plastic catheter
To moisten the exterior of the plastic catheter To ensure that the catheter’s suction is functioning properly
To ensure that the catheter’s suction is functioning properly To minimize friction as the catheter moves within the oral cavity
To minimize friction as the catheter moves within the oral cavity To avoid startling the patient with the sound created by the suction
To avoid startling the patient with the sound created by the suction
4. What is a priority intervention when performing oropharyngeal suctioning for a patient who is receiving oxygen by face mask?
 Complete the suctioning process in 20 seconds or less.
Complete the suctioning process in 20 seconds or less. Keep the oxygen mask near the patient’s face during the suctioning procedure.
Keep the oxygen mask near the patient’s face during the suctioning procedure. Encourage the patient to take several deep breaths before suctioning begins.
Encourage the patient to take several deep breaths before suctioning begins. Increase the oxygen flow rate by 1 L/min for 3 minutes before suctioning.
Increase the oxygen flow rate by 1 L/min for 3 minutes before suctioning.
5. Which action is most useful in evaluating the effectiveness of oropharyngeal suctioning?
 Comparing presuctioning and postsuctioning respiratory assessment data
Comparing presuctioning and postsuctioning respiratory assessment data  Confirming that the patient’s pulse oximetry value is >90%
Confirming that the patient’s pulse oximetry value is >90% Asking the patient to report any symptoms of dyspnea
Asking the patient to report any symptoms of dyspnea Assessing the patient’s skin for signs of cyanosis
Assessing the patient’s skin for signs of cyanosis
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

