Wound and Pressure Ulcer Care
Select a Skill:
- » Assessing Wounds
- » Irrigating Wounds
- » Changing a Dressing
- » Using Wound Drainage Systems
- » Caring for Pressure Ulcers
Take the Review Test:

Safety
- When a dry dressing inadvertently adheres to a wound, minimize trauma by moistening the gauze with sterile normal saline or sterile water before removing the dressing.
- In a moist-to-dry dressing, allow the inner primary dressing to dry and adhere to underlying tissues; moistening the dressing is a common error in technique that reduces the amount of debris the dressing removes.
- Discard solutions 24 to 48 hours after opening, and replace them with fresh solutions that are clearly labeled with the date and time of opening.
- Use sterile scissors to cut the amount of dressing needed to pack a wound. Pour the prescribed solution over the packing gauze or strip to moisten it. Do not let the strip touch the bottle. To avoid trauma during dressing removal, do not overpack the wound.
- If the wound appears inflamed and tender, begins draining, or has an odor, monitor the patient for signs of infection, notify the health care provider, and obtain a culture.
- If the wound bleeds during a dressing change, observe the color and amount of drainage. If it is excessive, apply a pressure dressing. Obtain vital signs as needed, and notify the health care provider.
- Use paper or nonallergenic tape, wraps, or mesh instead of adhesive tape in older adults. Adhesive can irritate their skin or cause it to tear.
Equipment
(Roll cursor over items to see labels)
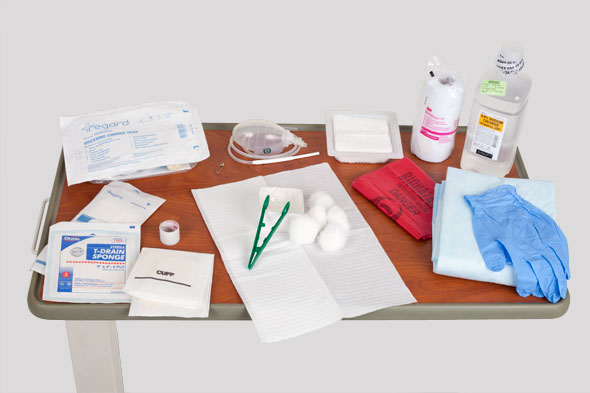
Clean gloves
Sterile normal saline
Sterile dressing kit
2 gauze pads
Sterile gloves
Cotton balls
Forceps
Sterile drape
Sterile basin (base of kit)
ABD dressing
Metapore tape
Wound drain (if needed)
Waterproof pad
Biohazard bag
Delegation
As the nurse, you are responsible for wound assessment and may not delegate this skill to nursing assistive personnel (NAP). In addition, you may not delegate the skill of caring for acute new wounds or any skills that require sterile technique or a moist-to-dry dressing change. You may, however, delegate the application of a dry dressing or a change of the top dressing. Be sure to inform NAP of the following:
- Review the signs of infection and poor wound healing. Instruct the NAP to report such findings to you immediately for further assessment.
- Explain any unique modifications, such as the need to use a special tape or taping technique to secure the dressing.
Preparation
- Assess the size and location of the wound.
- Determine the patient’s comfort level using a scale of 0 to 10.
- Assess the patient’s knowledge of the purpose of the dressing change.
- Assess whether the patient or a family member wishes to and is ready to participate in the dressing change.
- Review the medical orders for the dressing change procedure.
- Identify any risk factors for wound healing problems, including the following:
- Advanced age
- Prematurity
- Obesity
- Diabetes
- Compromised circulation
- Poor nutritional state
- Immunosuppressive drugs
- Irradiation of wound area
- High stress level
- Use of steroid medications
- Explain the procedure to the patient.
- When indicated, premedicate the patient 30 minutes before the dressing change with an ordered analgesic.
Follow-up
- Observe the appearance of the wound as it heals, including its size and the amount, color, and type of drainage. Note any erythema or swelling around the wound.
- Immediately report to the physician any problems or complications, such as drainage, an unexpected change in the appearance of the wound, accidental drain removal, bright-red bleeding, or signs of dehiscence or evisceration.
- Ask the patient to rate his or her pain using a scale of 0 to 10.
- Inspect the condition of the dressing at least once each shift.
- Ask the patient or a family member to describe the steps required for a proper dressing change.
Documentation
- Document the following:
- Appearance of the wound, including its color and the presence and characteristics of any exudate
- Any change in wound characteristics, especially a change in the amount of drainage
- Type and amount of dressings applied
- Patient’s tolerance of the dressing change
- Write the date and time of the dressing change in ink on a piece of tape, initial it, and affix the tape to the dressing. Do not use a marker.
- Report drainage, unexpected changes in the appearance of the wound, accidental drain removal, bright-red bleeding, or evidence of wound dehiscence or evisceration.
Review Questions
1. A patient complains of pain during a dressing change. What would be the most effective intervention the nurse could initiate at the next dressing change in order to reduce the patient’s pain?
 Premedicate the patient with a prescribed analgesic 30 minutes before the intervention.
Premedicate the patient with a prescribed analgesic 30 minutes before the intervention. Use a distraction technique to divert the patient’s attention during the procedure.
Use a distraction technique to divert the patient’s attention during the procedure. Position the patient comfortably before the intervention.
Position the patient comfortably before the intervention. Thoroughly explain the procedure to the patient.
Thoroughly explain the procedure to the patient.
2. Which action reduces the nurse’s risk for infection when changing the dressing of an infected abdominal wound?
 Begin antibiotic therapy before the dressing change.
Begin antibiotic therapy before the dressing change. Use appropriate personal protective equipment (PPE).
Use appropriate personal protective equipment (PPE). Adhere to sterile technique during the intervention.
Adhere to sterile technique during the intervention. Complete the dressing change in an effective, timely way.
Complete the dressing change in an effective, timely way.
3. What is the nurse’s best response when additional bloody drainage appears on the initial abdominal dressing of a patient who had surgery 7 hours ago?
 Notify the surgeon of the bleeding.
Notify the surgeon of the bleeding. Remove the dressing, and assess the wound.
Remove the dressing, and assess the wound. Assess the patient for signs of shock.
Assess the patient for signs of shock. Further assess the patient and the wound.
Further assess the patient and the wound.
4. When changing a patient’s surgical dressing 24 hours postoperatively, when would the nurse apply sterile gloves?
 After performing hand hygiene at the start of the procedure
After performing hand hygiene at the start of the procedure Before removing the inner dressing
Before removing the inner dressing After removing the original dressing materials and performing hand hygiene a second time
After removing the original dressing materials and performing hand hygiene a second time Just before cleansing the wound with sterile water
Just before cleansing the wound with sterile water
5. Which action would minimize the risk for cross-contamination while cleansing an infected abdominal surgical wound?
 Cleansing the wound with sterile water
Cleansing the wound with sterile water  Blotting the incision with dry gauze
Blotting the incision with dry gauze Wearing sterile gloves to cleanse the wound
Wearing sterile gloves to cleanse the wound Using a new gauze pad for each stroke while cleansing the wound
Using a new gauze pad for each stroke while cleansing the wound
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

