Wound and Pressure Ulcer Care
Select a Skill:
- » Assessing Wounds
- » Irrigating Wounds
- » Changing a Dressing
- » Using Wound Drainage Systems
- » Caring for Pressure Ulcers
Take the Review Test:

Safety
- Attach the drainage tubing to the patient’s gown with tape and a safety pin, so that the suction device is below the level of the wound and does not pull on the insertion site.
- Notify the health care provider of any signs of infection, including purulent drainage, odor, redness, increased white blood cell count, and temperature elevation.
- If bleeding appears in or around the drainage collector:
- Determine the amount of bleeding, and notify the health care provider if it is excessive.
- Assess for tension on the patient’s drainage tubing.
- Secure the tubing to prevent pulling and pain.
- If the drainage suction device is not accumulating drainage:
- Assess the drainage tubing for clots.
- Assess the drainage system for air leaks or kinks.
- Notify the health care provider.
- Take measures to prevent a confused patient from pulling out a drain collector.
Equipment
(Roll cursor over items to see labels)
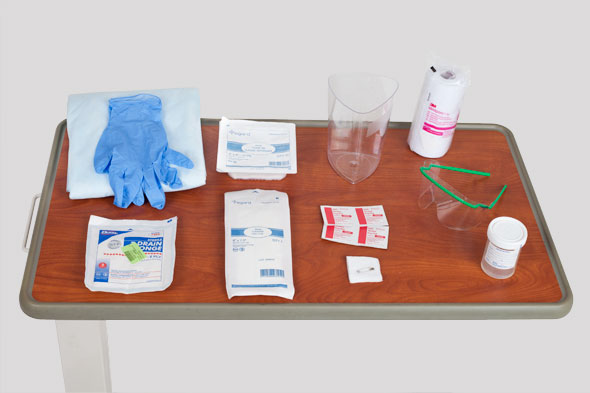
Graduated measuring cylinder
Alcohol swab
Gauze 4x4 split drain sponges
Goggles (optional)
Sterile specimen container
Sterile dressings:
- Gauze pads
- ABD bandage
Clean gloves
Safety pin
Metapore tape
Waterproof pad
Delegation
The assessment of wound drainage, the maintenance of drains, and the maintenance of drainage systems may not be delegated to nursing assistive personnel (NAP). However, the task of emptying a closed drainage container or pouch, measuring the amount of drainage, and recording the amount on the patient’s intake and output (I&O) record may be delegated. Be sure to inform NAP of the following:
- Discuss any modification of the skill necessary for the patient, such as increasing the frequency of drain emptying.
- Instruct NAP to report any change in the amount, color, or odor of drainage.
- Review the I&O procedure.
Preparation
- Identify the presence, location, and purpose of the closed-wound drain and drainage system as the patient returns from surgery. Assess any drainage on the patient’s dressing.
- Identify the type and number of wound drainage tubes and what each will be draining. Label each drain tube with a number or label.
- Check the health care provider’s orders to see if the drain tubes need self-suction, wall suction, or no suction.
- Inspect the system to determine the presence of one straight tube or Y-tube arrangement with two tube insertion sites.
- Inspect the system to ensure that it functions properly. This must include inspection of the insertion site, inspection of the drainage moving through the tubing in the direction of the reservoir, inspection of the patency of the drainage tubing and of the airtight connection sites, and inspection for the presence of any leaks or kinks in the system.
Follow-up
- Check for drainage in the suction device.
- Look for clots or large collections of debris that may block the flow of drainage. The Y site in the drainage tubing is especially prone to clogging.
- Inspect the wound for drainage, and look for seroma caused by accumulation of drainage fluid under the skin.
- Assess the patient’s level of comfort using a 0 to 10 scale.
Documentation
- Record emptying of the drainage suction device and the reestablishment of a vacuum in the suction device.
- Record the amount, color, and odor of drainage. Record the dressing change at the drain site and the appearance of the drain insertion site.
- Record the amount of drainage on the patient’s I&O record.
- Immediately report to the health care provider any sudden change in the amount of drainage, whether increased output or absence of drainage flow. Also report drainage with pungent odor, new evidence of purulence, severe pain, or dislodgment of the drainage tube.
Review Questions
1. What is the proper method for cleansing the evacuation port of a wound drainage system?
 Cleanse it with normal saline.
Cleanse it with normal saline. Wash it with soap and warm water.
Wash it with soap and warm water. Rinse it with sterile water.
Rinse it with sterile water. Wipe it with an alcohol sponge.
Wipe it with an alcohol sponge.
2. What is the nursing action to set up suction for a hemovac drainage system?
 Set the suction to lowest level possible.
Set the suction to lowest level possible. Hemovacs are always set to medium suction.
Hemovacs are always set to medium suction. Connect to the wall on intermediate suction.
Connect to the wall on intermediate suction. Compress the hemovac, creating suction.
Compress the hemovac, creating suction.
3. When emptying a Jackson-Pratt drain, which issue should nursing assistive personnel (NAP) report immediately to the nurse as a potential abnormality?
 The drainage is odorless.
The drainage is odorless. The drainage is straw colored.
The drainage is straw colored. The patient doesn’t like looking at the drainage tubing.
The patient doesn’t like looking at the drainage tubing. The amount of drainage was greater today than yesterday.
The amount of drainage was greater today than yesterday.
4. Which action might the nurse perform to ensure that the wound drainage tubing does not pull on the insertion site?
 Attach the tubing to the patient’s gown with a safety pin.
Attach the tubing to the patient’s gown with a safety pin. Tape the tubing to the patient’s bed.
Tape the tubing to the patient’s bed. Attach the tubing to the nearest side rail.
Attach the tubing to the nearest side rail. Loop the tubing through the bed frame.
Loop the tubing through the bed frame.
5. Which action would maximize the suction produced by the Jackson-Pratt drainage system after the system has been emptied?
 Pinning the tubing to the patient’s hospital gown
Pinning the tubing to the patient’s hospital gown Compressing the bulb while replacing the port cap
Compressing the bulb while replacing the port cap Emptying the drainage container only when it is 90% full
Emptying the drainage container only when it is 90% full Placing the drainage container below the wound site
Placing the drainage container below the wound site
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

