Wound and Pressure Ulcer Care
Select a Skill:
- » Assessing Wounds
- » Irrigating Wounds
- » Changing a Dressing
- » Using Wound Drainage Systems
- » Caring for Pressure Ulcers
Take the Review Test:

Safety
- Patients who have altered mobility are considered at risk for developing pressure ulcers.
- Minimize friction and shear by use of lift sheets when repositioning patients; raise the head of the bed no more than 30 degrees (unless medically contraindicated) to prevent sliding and shear injury.
- Impaired skin at the edge of the ulcer indicates progressive tissue damage. Maceration on the periwound skin indicates the need to select a new type of wound dressing.
- When treating an ulcer, make sure the absorbency of the dressing is adequate for the wound drainage. Check to ensure that the wound does not dry out and that the surrounding skin does not macerate.
- Inspect your patient’s skin at least daily. Examine all pressure points, and document your findings.
- If the ulcer becomes deeper, with increased drainage and/or development of necrotic tissue:
- Review current wound-care management.
- Consult with the multidisciplinary team regarding changes in the wound-care regimen.
- Obtain wound cultures.
Equipment
(Roll cursor over items to see labels)
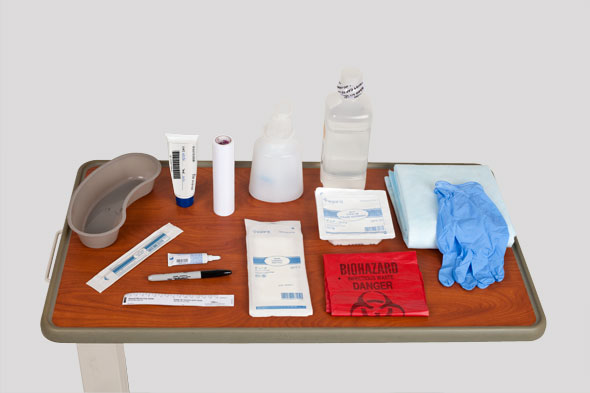
Clean gloves
Biohazard bag
Wound measuring device
Sterile cotton-tipped applicators
Topical agent
Enzyme
Sterile normal saline
Sterile container and 60 cc syringe
Sterile 4x4 gauze pads
Permanent marker
ABD dressing
Metapore tape
Waterproof pad
Emesis basin
Delegation
The skill of changing a pressure ulcer dressing may not be delegated to nursing assistive personnel (NAP). Delegation of related skills varies by state Nurse Practice Act. Be sure to inform NAP of the following:
- Report any wound drainage on linens or intact skin. This would indicate a need to change the dressing or to use an alternative dressing.
- Report any new areas of redness, blistering, or skin irritation.
- Reposition the patient comfortably every 2 hours.
Preparation
- Assess the patient’s level of comfort and need for pain medication. Assess the patient for the following factors: complications and comorbidities, nutritional adequacy, presence and severity of pain, psychosocial factors, and risk for additional pressure ulcers.
- Assess the patient and the caregiver’s understanding of prevention, treatment, and factors that contribute to the recurrence of pressure ulcers.
- Explain the wound care procedure to the patient and family caregiver. Individualize the teaching plan for an older adult patient, taking into account the normal aging changes that affect learning.
Follow-up
- Observe the skin surrounding the ulcer for inflammation, edema, and tenderness.
- Inspect the dressings and exposed ulcers for drainage, foul odor, and tissue necrosis. Monitor the patient for signs of infection including fever and an elevated white blood cell (WBC) count.
- Compare subsequent ulcer measurements using one of the scales designed to measure wound healing, such as the ASEPSIS Tool, PUSH Tool, or BWAT.
Documentation
- Record the following:
- Type of wound tissue present in the ulcer
- Ulcer measurements
- Periwound skin condition
- Character of drainage or exudate
- Type of topical agent used
- Type of dressing applied
- Patient’s response
- Report any deterioration in the appearance of the ulcer to the nurse in charge or the health care provider.
Review Questions
1. Which practice protects the nurse from infection when changing the dressing on an infected pressure ulcer?
 Begin antibiotic therapy before the dressing change.
Begin antibiotic therapy before the dressing change. Use appropriate personal protective equipment.
Use appropriate personal protective equipment. Adhere to sterile technique during the intervention.
Adhere to sterile technique during the intervention. Complete the dressing change in an effective, efficient manner.
Complete the dressing change in an effective, efficient manner.
2. The wound bed of a patient’s pressure ulcer is red. What does this finding indicate to the nurse?
3. Which measurements would the nurse use to calculate the surface area of a patient’s pressure ulcer?
4. How would the nurse safely apply an enzyme debridement ointment?
 Daub ointment on dead tissue at the wound edges.
Daub ointment on dead tissue at the wound edges. Put ointment on a tongue blade, and gently spread it on the center of the wound.
Put ointment on a tongue blade, and gently spread it on the center of the wound. Apply ointment to necrotic tissue in the wound while avoiding contact with surrounding skin.
Apply ointment to necrotic tissue in the wound while avoiding contact with surrounding skin. Apply a gauze dressing to ensure contact with the ointment.
Apply a gauze dressing to ensure contact with the ointment.
5. Which action can the nurse delegate to nursing assistive personnel (NAP) to help prevent the development of pressure ulcers in an older adult patient?
 Reposition the patient at least every 2 hours.
Reposition the patient at least every 2 hours. Assess the patient’s bony prominences every shift.
Assess the patient’s bony prominences every shift. Educate the family about the importance of healthy skin.
Educate the family about the importance of healthy skin. Assist the patient in the selection of high-protein foods.
Assist the patient in the selection of high-protein foods.
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

